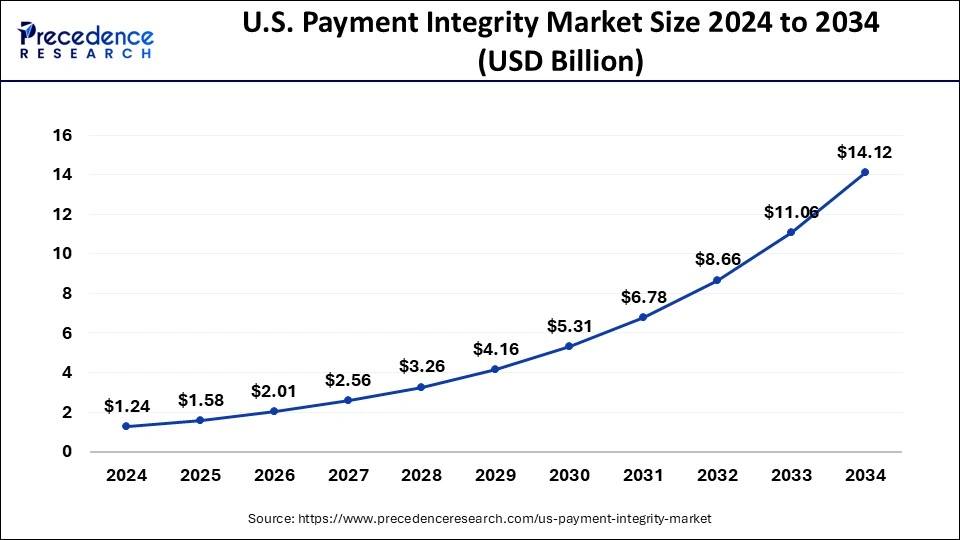
The U.S. payment integrity market size reached USD 0.98 billion in 2023 and is predicted to hit around USD 10.27 billion by 2033, growing at a CAGR of 26% during the forecast period from 2024 to 2033.
Payment integrity is critical for healthcare providers because it ensures accurate and timely compensation. The National Healthcare Anti-Fraud Association estimates that healthcare fraud costs around 3% of overall healthcare expenses. Payment integrity programs target fraud and inefficient billing practices, such as accurate party identification, membership eligibility, and contractual compliance.
Providers must be aware of payers’ attempts to combat fraud and compliance concerns. Ensuring payment integrity requires robust documentation and coding processes, as well as education. Clear documentation rules, documentation templates in electronic health records (EHR), and computer-assisted coding systems can all aid with coding procedures.\
Get a Sample: https://www.precedenceresearch.com/sample/3060
U.S. Payment Integrity Market Revenue (USD Million) 2022-2032, By Component
| By Component | 2022 | 2023 | 2027 | 2032 |
| Software | 486.52 | 618.38 | 1,626.54 | 5,545.27 |
| Services | 285.74 | 361.62 | 934.94 | 3,119.22 |
U.S. Payment Integrity Market Revenue (USD Million) 2022-2032, By Function
| By Function | 2022 | 2023 | 2027 | 2032 |
| Query & Reporting | 270.29 | 342.51 | 890.11 | 2,989.25 |
| OLAP & Visualization | 308.9 | 392.98 | 1,037.4 | 3,552.44 |
| Performance Management | 193.07 | 244.51 | 633.97 | 2,122.8 |
U.S. Payment Integrity Market Revenue (USD Million) 2022-2032, By Application
| By Application | 2022 | 2023 | 2027 | 2032 |
| Pre-payment | 193.07 | 247.94 | 678.79 | 2,426.06 |
| Post-payment | 386.13 | 488.04 | 1,255.12 | 4,158.95 |
| FWA | 154.45 | 195.51 | 505.89 | 1,689.58 |
| Others | 38.61 | 48.51 | 121.67 | 389.9 |
U.S. Payment Integrity Market Key Insights
- By component, the software segment has held a major revenue share of 63.10% in 2023.
- By function, the OLAP & visualization segment has contributed 40.10% of revenue share in 2023.
- By application, the post-payment segment has recorded the largest revenue share of 49.80% in 2023.
- By mode of delivery, the on-premises segment has generated more than 55.95% of revenue share in 2023.
- By end-use, the healthcare providers segment has captured more than 64.75% of revenue share in 2023.
U.S. Payment Integrity Market Segments Outlook
Component Outlook
The software segment dominated the U.S. payment integrity market in 2023. Payment integrity (PI) is critical in US healthcare, as it ensures accurate claims adjunction and appropriate compensation for service delivery. To address basic problems and examine difficult situations, software and analytics technologies, as well as coding specialists and medics, are used. Services are delivered by corporate health plan departments and specialist PI businesses.
Payment processing software automates transactions on different platforms by connecting with shopping carts, accounting software, and customer relationship management systems. The market is competitive, with several high-quality solutions, necessitating careful evaluation of unique company requirements when picking a platform.
Function Outlook
The OLAP & visualization segment dominated the U.S. payment integrity market in 2023. Online analytical processing (OLAP) provides data engineers and analysts with five major advantages: better decision-making, increased data visualization, time savings, flexibility, and a competitive edge. There are three types of OLAP systems: multidimensional (MOLAP), relation (ROLAP), and hybrid (HOLAP). ROLAP systems employ relational databases for data storage and SQL queries, but MOLAP stores data in a multidimensional cube structure that allows for complicated computations and aggregations.
HOLAP combines the best features of both systems, allowing users to store summary data in multidimensional cubes and specific business data in a relational database. The type of OLAP system used is determined by the organization’s unique analytical requirements, such as data complexity, query response time, and analysis and reporting.
Application Outlook
The post-payment segment dominated the U.S. payment integrity market in 2023. Post-payment changes are critical for ensuring compliance and accuracy in healthcare reimbursement. They include thorough audits, payment reconciliation, benefits coordination, subrogation, and overpayment recovery. These procedures assist in detecting fraud, ensuring genuine claims, preventing financial overlaps, and ensuring appropriate reimbursement from providers.
Mode of Delivery Outlook
The on-premises segment dominated the U.S. payment integrity market in 2023. On-premises is a conventional approach to delivering and maintaining hardware and software on a company’s premises. It provides total control over IT infrastructure, customization, and local data storage, especially for sensitive or secret information. It also allows for faster access to data.
On-premises software, on the other hand, can be expensive to implement and maintain since it requires hardware and software licensing. Scaling up on-premises infrastructure may be difficult and time-consuming. Despite these issues, on-premises software is still a viable choice for firms that can afford to acquire and maintain licenses.
End Use Outlook
The healthcare providers segment dominated the U.S. payment integrity market in 2023. Payment integrity in healthcare is a method that seeks to detect faults, duplication, and inconsistencies that patients would have paid for, resulting in cost-cutting solutions. It also tries to stop unfair invoicing practices in the future.
Despite industry customs, payment integrity prioritizes accountability over convention. It seeks to restore the balance of power to some semblance of equality, notwithstanding the seeming extreme upheaval caused by minor administrative adjustments.
U.S. Payment Integrity Market Scope
| Report Coverage | Details |
| Market Size in 2023 | USD 0.98 Billion |
| Market Size by 2033 | USD 10.27 Billion |
| Growth Rate from 2024 to 2033 | CAGR of 26% |
| Base Year | 2023 |
| Forecast Period | 2024 to 2033 |
| Segments Covered | By Component, By Function, By Application, By Mode of Delivery, and By End Use |
U.S. Payment Integrity Market Dynamics
Drivers
Cost savings
Payment integrity can result in significant cost reduction by reducing fraudulent claims, billing mistakes, and inefficient practices. This can cut wasteful spending by 8% to 10% or more, guaranteeing effective resource allocation and high-quality patient care. Healthcare fraud costs the US tens of billions of dollars every year. Advanced data analytics and predictive modeling can assist payers in detecting and preventing fraudulent activity, leading to considerable cost savings.
Enhanced provider-payer relationship
Payment integrity solutions help healthcare providers and payers build stronger relationships by offering clear rules and instructional materials. This partnership speeds claim processing, lowers mistakes, and increases efficiency.
Providers who understand payment integrity submit more accurate claims, which reduces the need for adults and appeals. This results in speedier reimbursement and more dependable care, which benefits patients by assuring timely access to high-quality care, boosting the growth of the U.S. payment integrity market.
Restraint
Billing errors
Payment integrity is difficult to maintain owing to billing errors and erroneous claims caused by coding errors, paperwork discrepancies, or misconceptions of reimbursement criteria. These mistakes might cause healthcare providers to be overpaid or underpaid, resulting in financial inaccuracies and conflicts.
Inefficiencies in claims processing, such as manual processes, a lack of defined protocols, and complex reimbursement systems, can also cause delays, mistakes, and higher administrative expenses, affecting the entire healthcare payment ecosystem.
Read Also: Semiconductor Market Size to Hit USD 1,137.57 Billion by 2033
Opportunity
AI-based technology
Payment integrity is evolving toward prepaid solutions and AI-powered interventions, with the latter used earlier in the claim lifecycle to save costs. As the complexity of payment integrity solutions increases, health plans will need platform-based techniques to easily integrate and model the impact of varied capabilities. In terms of product design and deployment tactics, successful suppliers promote flexibility and customer-centricity.
Advanced Large Language Models can transform payment integrity and patient engagement by facilitating more natural interactions and individualized support. The confluence of AI and prepay editing solutions is resulting in unparalleled accuracy, value development, and transparency throughout the healthcare industry. Technology partners will play an important role in simplifying the business of care and allowing more efficient, effective, and equitable healthcare.
U.S. Payment Integrity Market Companies
- Cotiviti
- Optum / Change Healthcare
- Zelis
- Availity
- MultiPlan
- Ceris
- Cognizant
- EXL
- Performant
- Syrtis
- Varis
- ClarisHealth
- ClaimLogiq
- Rialtic
- HealthEdge
Recent Developments:
- In May 2024, Penstock Group obtained HITRUST accreditation for ClearBridge, their SaaS payment integrity solution. ClearBridge’s two-year accreditation indicates compliance with regulatory and industry requirements, as well as risk management. This accreditation ranks Penstock among the few global firms that have obtained it, proving the HITRUST Assurance Program’s rigorous security measures.
- In May 2024, Zelis, a prominent healthcare technology supplier, launched the Zelis Advanced Payments Platform (ZAPP) to help simplify the processing of large amounts of claims payments and technical needs. The platform intends to streamline operations, decrease complexity, and assure compliance with technology, regulatory requirements, and customer expectations, all while offering a payment experience that caters to both providers and members.
